A wet tile near the sink can feel harmless until a heel slides half an inch. Many older adults learn that lesson fast, especially when balance is already a daily effort. Families often start planning after a scare, not after a clean and dramatic emergency. That timing makes clear thinking harder, because fear tends to drive rushed choices.
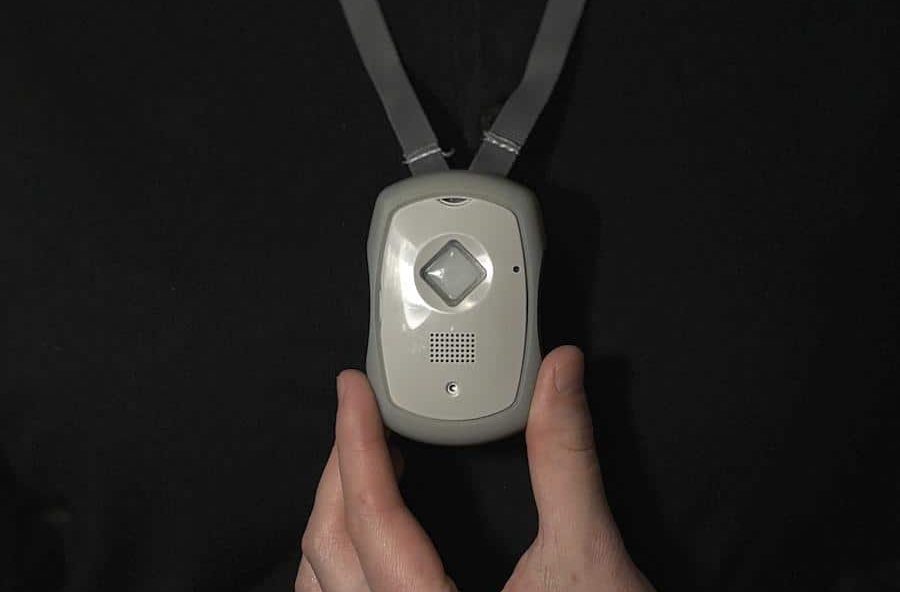
A medical alert necklace can make daily life safer without turning it into a supervised routine. When it fits well and the plan is clear, a senior can keep doing normal things, showering, walking to the mailbox, running errands, while still having a simple way to get help quickly. The right choice is less about flashy features and more about wear habits, water use, fall detection expectations, and privacy settings that protect the senior’s control.
Start With Real Risk, Not A Generic Checklist
Most home emergencies start during normal tasks, like carrying laundry or stepping off a curb. Falls are common later in life, and delayed help can raise the chance of complications. Start by listing the rooms where the senior spends time alone, including entryways and bathrooms. Then note poor lighting, loose rugs, and stairs that do not have a sturdy handrail.
A short risk list also includes health triggers that raise odds of a fall or fainting. Blood pressure changes, medication side effects, and low vision can change safety in one week. If memory is uneven, add situations where a phone may be forgotten or left charging. Those are the moments where a wearable option tends to matter most.
To keep the plan grounded, write down three “most likely” scenarios and one “worst day” scenario. That might be a shower slip, a dizzy spell while cooking, or a stumble outside the mailbox. Then match features to those situations, so the device has a clear job each day. For fall risk context, the CDC’s falls page is a useful starting point.
Comfort And Wear Habits Decide Everything
A device that is not worn cannot help, even if the monitoring service is excellent. Comfort problems are common, especially with sensitive skin, sweaters, and winter collars. Ask the senior how they feel about necklaces, because some people remove them at home. That habit matters more than any technical promise printed on a product page.
Test comfort during a normal day, not just for thirty seconds at a kitchen table. Try it with a coat, a scarf, and a seatbelt, then notice any pulling or pinching. If the necklace catches on clothing, it will end up on a dresser by day three. A slightly simpler device worn daily can beat a feature heavy device left behind.
It also helps to talk about pride, because many seniors dislike “medical looking” gear. A discreet style can make daily wear easier, without changing safety goals. Ask whether the clasp is easy for stiff fingers, or if it needs caregiver assistance. If setup feels frustrating, the senior may resist wearing it without saying why.
Fall Detection And Water Use Need Clear Expectations
Fall detection can help when someone cannot press the help button after a hard drop. Still, automatic detection is not magic, and it can miss slow slides or unusual angles. False alarms can also happen during quick chair drops, brisk dancing, or a heavy cough. That does not make the feature bad, it just means expectations should be realistic.
Ask how the system confirms an event, and what happens if the wearer cannot answer. Some services try two way voice first, then move to emergency contacts if needed. Clarify whether the alert will still be treated as urgent when there is no response. This matters most for seniors who live alone, or who may freeze during stress.
Water use is another area where real life details matter more than a marketing label. Many falls happen in bathrooms, and shame can stop a person from calling for help. Confirm that the device is water resistant enough for showers, not only quick splashes. Then check whether the cord feels comfortable on wet skin for ten minutes or longer.
Monitoring And Response Planning Reduce Confusion
Monitoring sounds simple until an actual alert happens at 2:10 a.m. on a weekday. In that moment, a clear script matters more than vague reassurance and general promises. Families should confirm the call order, because assumptions often differ between siblings. Write it down, then share it, so nobody debates during an emergency.
Two way voice can help seniors who feel disoriented after a fall or sudden pain. It can also reduce panic, because a calm voice can guide breathing and simple checks. Still, response speed depends on setup accuracy, including address, unit number, and entry details. If a building has a gate code, include it, or responders may lose minutes outside.
A simple checklist keeps this part practical, and it makes reviews easier every few months.
- Confirm who gets called first, and who is called only if the first person cannot answer.
- Record allergies, mobility limits, and preferred hospital, if that preference is medically reasonable.
- Note language needs, hearing issues, and whether the senior uses a walker or cane daily.
- Recheck the plan after any move, medication change, or new caregiver schedule.
Privacy, Consent, And Family Roles Matter In Canada
Emergency monitoring can involve health details, location information, and recorded call notes. That raises privacy questions, especially when adult children manage accounts for a parent. The safest path is a clear consent conversation while the senior feels calm and in control. This protects dignity, and it also reduces family conflict later.
Start with preferences, not pressure, and let the senior name what feels acceptable. Ask who should be contacted first, and what information can be shared with each person. Then document those choices in a simple written note that everyone can access quickly. Even a one page summary can prevent arguing during a stressful night.
If a senior already has a power of attorney, align device access with that document. If not, families may need to discuss legal planning before a crisis forces quick decisions. The National Institute on Aging has a practical legal planning guide. That kind of preparation can reduce confusion when medical decisions happen fast.
Finally, review what the service stores, who can view it, and how updates are handled. Confirm how contact lists are changed, and whether the senior can approve changes each time. If multiple relatives share responsibility, set one account manager to reduce messy edits. Clear roles help everyone support safety without turning care into constant monitoring.
Getting The Choice Right Without Overthinking It
A good choice is the one the senior will wear daily, with a response plan everyone understands. Match fall detection and water use to real routines, then write down contact order and consent details. When comfort, expectations, and privacy are clear, emergencies become less chaotic and more manageable. That is the real goal, quick help without stripping a person of normal independence.